T-cells aimed at most tumours
 Scientists in the US have used engineered T-cells to attack tumours.
Scientists in the US have used engineered T-cells to attack tumours.
The researchers say their new technique can arrest tumor growth for a variety of cancers and squash the spread of cancer to other tissues.
“I think the beauty of what we've been involved in is that it expands the scope of immunotherapy,” says research leader Dr Paul Fisher from the Virginia Commonwealth University.
“Our approach is less dependent on cancer cells expressing something specific to target.”
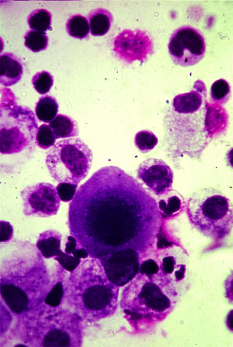
Previous studies have led to the creation of the now commercially-available chimeric antigen receptor T (CAR-T) cell therapy, which is designed to destroy cancer cells expressing specific surface molecules.
But CAR-T has made limited progress on solid tumors, such as prostate cancer or melanoma, because the cells that make up those tumors are not all the same, which blocks the engineered T-cells from recognising and attacking.
Dr Fisher discovered a protein called IL-24 that attacks a variety of cancers in several different ways.
In the latest study, his team was able to deliver the gene coding for IL-24, which is called MDA-7, to solid tumors using T-cells.
Engineering T cells to produce MDA-7/IL-24 allows killing of cancer cells regardless of their expression of target molecules.
At the sub-cellular level, MDA-7/IL-24 binds to receptors on the surface of cells and instructs them to make and release more copies of the MDA-7/IL-24 protein. If the cell is normal, the protein is simply secreted and no damage occurs.
However, if the cell is cancerous, MDA-7/IL-24 causes oxidative stress damage and ultimately cell death, not only within the primary tumor but also among its distant metastases - the cause of death in 90 per cent of patients.
As a result of this process, the immune system generates memory T-cells that can theoretically kill the tumour if it ever comes back.
At the whole tumor level, IL-24 also blocks blood vessel formation, starving tumors of the nutrients needed to sustain their unchecked growth.
In mice with prostate cancer, melanoma or other cancer metastases, MDA-7/IL-24-expressing T cells slowed or stopped cancer progression better than unmodified T cells.
The researchers also discovered that arming T cells with MDA-7/IL-24 allowed them to survive better and multiply in the tumor microenvironment - the space right around the cancerous mass.
In the clinic, this approach would involve extracting the patient's own T-cells from tumor samples, genetically engineering them to express MDA-7/IL-24, growing millions of copies of the cells in the lab and finally transplanting them back into the patient.
The experts say the procedure could be carried out in a way that is generally safe and minimally invasive.
Clinical trials using different methods of delivering IL-24 are already underway for several cancers.
The researchers say they are working to optimise their technology for the treatment of solid tumors and cancer metastases, in anticipation of future human trials.







 Print
Print