Cell 'armour' helps
 Researchers have developed a kind of cellular ‘armour’ to improve cancer therapies.
Researchers have developed a kind of cellular ‘armour’ to improve cancer therapies.
A new study from the University of Pennsylvania unveils a game-changing innovation to enhance the safety of chimeric antigen receptor T cell (CAR T) therapy.
CAR T therapy, hailed as a beacon of hope in recent years, holds immense potential in combating various cancer types by genetically modifying patients' T-cells to combat malignant cells.
However, its application has been marred by severe and sometimes fatal side effects, including cytokine release syndrome (CRS) and neurotoxicity.
Despite the US FDA's green light for six CAR T therapies and several others in the pipeline, the grim spectre of CRS and neurotoxicity has been an insurmountable obstacle to broader clinical implementation.
Enter Michael Mitchell, an associate professor at the University of Pennsylvania's School of Engineering and Applied Science, and his team, whose groundbreaking findings published in the journal Nature Materials present a promising solution.
“The complex challenge of addressing CRS and neurotoxicity without compromising CAR T cell effectiveness has perplexed researchers,” he says.
“Unwanted interactions between CAR T cells and immune cells called macrophages drive overactivation, leading to the release of toxic cytokines.”
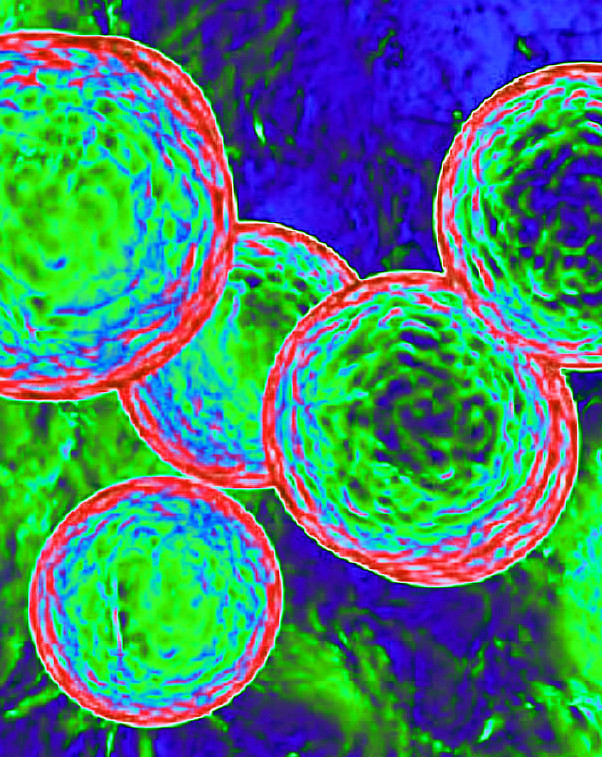
The proposed solution is a materials engineering-based strategy that involves affixing a sugar molecule to the surface of CAR T cells.
These sugar molecules act as reactive handles, enabling the creation of a biomaterial coating inside the body. This ‘suit of armour’ effectively shields CAR T cells from dangerous macrophage interactions.
“We attached this sugar molecule to the CAR T cells using metabolic labelling. This modification enables the CAR T cells to attack cancer cells without any hindrance,” says Ningqiang Gong, the study's first author,.
Remarkably, this approach not only safeguards patients but also opens a new therapeutic window.
As the PEG on CAR T cells gradually dilutes, interactions with tumour cells are restored before interactions with macrophages.
This restoration permits CAR T cells to target and eliminate cancer cells without inducing macrophage overactivation, thus mitigating the risk of severe CRS and neurotoxic effects. By incorporating the PEG buffer, the team says it has successfully modulated CAR T cell-macrophage interactions, creating a safer and more effective therapy.
The implications of this research extend beyond safety nets for patients; the team envisions broader applications, including other cellular immunotherapies.
More details are accessible here.








 Print
Print