CHRIS aids COVID response
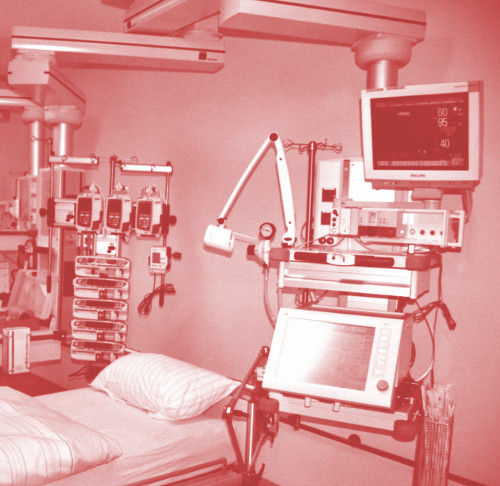 Developers say that a high-tech ICU monitoring tool saved lives in Victoria’s COVID-19 second wave.
Developers say that a high-tech ICU monitoring tool saved lives in Victoria’s COVID-19 second wave.
Dr David Pilcher, an intensivist at the Alfred Hospital in Melbourne, has detailed the development and success of the Critical Health Resources Information System (CHRIS).
“In late March 2020, rising numbers of COVID-19-related admissions to ICUs (intensive care units) were observed throughout Australia,” Dr Pilcher says.
“ANZICS and the Australian Government Department of Health recognised that ICU demand was unlikely to be uniform, that capacity might be exceeded in one region but not in another, and that matching ICU resources to areas of greatest need might be required.
“A single sentence encapsulated the approach: ‘Why would we let a patient die in Western Australia if we can see a spare ventilator in Sydney?’”
In a collaboration between ANZICS, the DoH, Telstra Purple and Ambulance Victoria, a national dashboard of ICU activity (CHRIS) was created.
“All adult and paediatric ICUs (public and private) in Australia were instructed to enter data twice daily,” Dr Pilcher says.
“Each ICU was immediately able to see patient numbers and resources available within every ICU in their region and also see an aggregate summary of all ICUs in Australia.
“CHRIS was available to all state and territory health departments, to all patient transport and retrieval agencies, and also to ICUs in New Zealand.
“The system went live on 1 May 2020, after 26 days of development. Three weeks later, 184 out of 188 eligible ICUs (98 per cent) in Australia were contributing data.”
When the second wave of COVID-19 hit Melbourne and Victoria at the end of June 2020, CHRIS was ready to assist.
“From the beginning of July to the end of September 2020, there were 237 ICU admissions with COVID-19 pneumonitis, of which 210 (88 per cent) occurred in July and August,” Dr Pilcher wrote.
“Admissions were predominantly to public hospitals in north-western Melbourne.
“The rapid and localised nature of presentations meant that it was faster to transfer patients to ICUs with vacant capacity than to open and staff additional beds, despite physical ICU bed spaces being available.
“Transfers from the emergency department or ICU at the four north-western metropolitan hospitals alone accounted for 35 per cent (46/133) of all critical care transfers in Victoria during July and August.
“Spare ventilators were available at all sites on all days.”
CHRIS provided real-time data on ICU activity and capacity, as well as facilitating the transfer of critically ill patients.
“CHRIS also enabled early diversion of ambulance presentations to emergency departments at hospitals where ICUs had capacity,” Dr Pilcher says.
“These approaches were integral to ensuring standards of care were maintained by clinicians, retrieval agencies and the Victorian health department.
“At the same time, there was visibility to the Australian Government Department of Health, which would, if required, coordinate a national response to overwhelmed ICU services.”
CHRIS has the potential to be used beyond intensive care settings, the experts say.
“The tool may also assist in the response to local and national public health emergencies, such as mass casualty events, bushfires or thunderstorm asthma,” Dr Pilcher concludes.
“Automated linkage of CHRIS to existing state-based and national systems should be investigated. In addition, it may have potential use in monitoring health policy impacts more broadly.”








 Print
Print