DVT study urges closer view
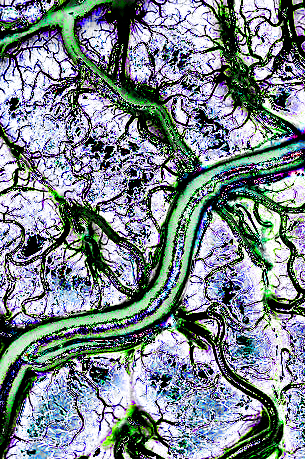 Doctors are being urged to keep a careful eye on deep vein thrombosis, a difficult-to-spot but potentially deadly condition.
Doctors are being urged to keep a careful eye on deep vein thrombosis, a difficult-to-spot but potentially deadly condition.
New research has found that clinical presentation of DVT is often “non-specific” and accurate diagnosis requires careful integration of clinical assessment, evaluation of pre-test probability and objective diagnostic testing.
Professor Graeme Hankey, a world-leading expert on stroke research from the University of Western Australia, said signs and symptoms of DVT include localised pain, swelling, redness and dilated veins close to the surface of the skin.
The researchers said anticoagulation remains the gold standard treatment for DVT.
“The choice of anticoagulant should consider medical issues such as efficacy, safety, renal and hepatic function, and concurrent medications,” Professor Hankey said.
“In addition, practical issues such as availability, familiarity of use, patient preference and cost should be considered.”
Compression stockings have been shown to have a beneficial effect after diagnosis. In rare cases, devices to stop blood clots, treatment to dissolve blood clots or surgery to remove blood clots may be considered.
Situations which are likely to impact the choice of anticoagulant agent and duration of treatment include DVT which occurs in pregnant women, patients with cancer, DVT of the lower leg, recurrent DVT, autoimmune disorders such as antiphospholipid syndrome or those with superficial vein thrombosis, Professor Hankey said.
“The diagnosis of DVT requires a high index of suspicion because symptoms and signs are often non-specific,” he said.
“Anticoagulation continues to be the cornerstone of therapy. The optimal anticoagulant and duration of therapy are determined by the clinical assessment.”








 Print
Print