Experts study COVID echoes
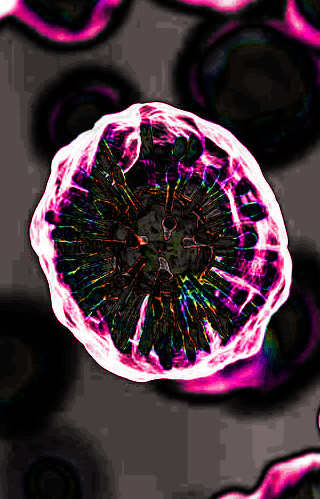 Australian experts have delivered crucial insight into the lasting immune system dysregulation caused by COVID-19.
Australian experts have delivered crucial insight into the lasting immune system dysregulation caused by COVID-19.
A new study shows that people’s immune systems can be significantly altered 6 months after their COVID- 19 infection.
The immune cells and gene expression experienced during this post-infection period holds clues to the intriguing ‘Long COVID’ symptoms affecting some patients.
The immune systems of 69 participants between 20 and 80 years of age were examined over a 6-month period, following infection with the original strain of SARS-CoV-2, the virus that causes COVID-19.
Of the total cohort, 47 were recovering from mild infection, 6 from moderate and 13 were recovering from severe or critical COVID-19 disease.
The unique longitudinal analysis examined antibody responses, the expression of thousands of genes in the blood, and approximately 130 different types of immune cells, via blood samples taken at 12, 16 and 24-weeks post infection. Responses were compared to healthy controls.
Professor David Lynn says the results show that the immune system of people previously infected with SARSCoV- 2 was significantly altered until at least 6 months post-infection.
“The study found substantial dysregulation of immune cell numbers that was strongest at 12-weeks post infection but was still evident in most cases for up to 6 months and potentially even longer,” Prof Lynn said.
In addition to an increased number of immune cells and antibodies, there was also strong dysregulation of gene expression, particularly in those genes linked to inflammation. Gene expression refers to information stored in DNA that regulates how cells respond to changing environments.
This can include controlling when and how much response is made against an invading virus.
Professor Simon Barry says deep immunophenotyping will develop the understanding of how rare immune cells help repair the damage and set up immunity to COVID-19.
“By taking a deep dive into the immune cells in these patients, we’ve found some new players linked to the disease, and these may help understand why some people have more severe disease, or get Long COVID,” he said.
The reason why some individuals are so harshly affected by Long COVID, while others are barely affected, remains a mystery.
“At present there are no treatments for Long COVID sufferers and as the world slowly transitions to living with COVID, we will need to find answers and better solutions to prevent and treat Long COVID in the years to come” said Dr Branka Grubor-Bauk.
Surprisingly, the research did not find a strong correlation between severity of infection and the severity of immune dysregulation post infection. Immune dysregulation was evident even in those patients who experienced mild infection.
“We’ve seen a very broad spectrum in the rate of recovery and we still don’t understand why some people are recovering so much quicker than others,” Prof Lynn said.
“The level of disease severity doesn’t translate directly to the level of immune dysregulation and we haven’t been able to find any patterns indicating that an individual’s age or sex is a differentiating factor governing differences in recovery. Clearly there are other factors at play that need to be explored.”








 Print
Print