Study shows diabetic cell success
 In an exciting breakthrough for diabetics, researchers have created insulin-making pancreas cells in a dish.
In an exciting breakthrough for diabetics, researchers have created insulin-making pancreas cells in a dish.
The lab grown cells were able to produce insulin and respond to sugar, and when they were transplanted into diabetic mice the cells produced insulin in response to glucose spikes in the blood.
The team behind the work says it could lead to the development of patient-specific insulin-producing cells that could be transplanted into people with diabetes.
Previously, when human stem cells develop into beta cells in a dish, they only reach a precursor stage, unable to fully mature, so they cannot effectively produce insulin in response to glucose.
Now, scientists have discovered a protein that activates the maturation process in vitro, overcoming this longstanding obstacle in diabetes therapy development.
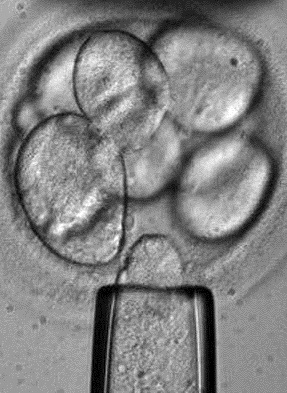
To create different cell types in the lab, stem cells are pushed into determination - the paths young cells normally travel to become neurons, skin cells, muscle cells, or any number of other cell types.
However, there are many developmental points between a stem cell and a fully grown cell type, and for pancreatic beta cells, the stem cells have historically stalled in an early stage when grown in the lab.
To get to the adult beta cells and find out what triggers the next step in the process, the team analysed human cells' transcriptomes.
Here, they discovered that a nuclear receptor protein - estrogen-related receptor γ (ERRγ) - occurred in large amounts in adult beta cells.
“In muscle, ERRγ induces greater mitochondrial growth and promotes oxidative use of sugars and lipids to generate energy,” says researcher Ronald Evans, a molecular biologist.
“It was a little bit of a surprise to see that beta cells produce a high level of this regulator, but beta cells have to release massive amounts of insulin quickly to control sugar levels. It's a very energy-intensive process.”
When the researchers raised mice that lacked ERRγ, the animals' beta cells did not produce insulin in response to blood glucose spikes.
But when the team instructed human beta-like cells grown in the lab to produce more ERRγ; “Voilà”, says Evans.
“Those cells in culture began to respond to glucose and release insulin.”
To further test the dish-matured cells, the researchers transplanted them into diabetic mice.
From the first day of transplantation, the cells produced insulin in response to glucose spikes in the mice's blood, alleviating the modelled diabetes.
“We were very excited when we saw that,” says Evans.
Turning on the ERRγ switch alone is sufficient to mature the beta-like cells in vitro, with the power to rescue diabetes in vivo, the team concludes.
“I believe this work transitions us to a new era in creating functional beta cells at will,” says Evans.
The researchers are planning to explore this process in more complicated models for treating diabetes.
The study is accessible here.








 Print
Print