Thin bug killer scores well
 Australian researchers have invented a nano-thin superbug-slaying material.
Australian researchers have invented a nano-thin superbug-slaying material.
The material is designed to one day be integrated into wound dressings and implants to prevent or heal bacterial infections.
The innovation - which has undergone advanced pre-clinical trials - is effective against a broad range of drug-resistant bacterial cells, including ‘golden staph’, which are commonly referred to as superbugs.
Antibiotic resistance is a major global health threat, causing about 700,000 deaths annually, a figure which could rise to 10 million deaths a year by 2050 without the development of new antibacterial therapies.
A new study led by RMIT University and the University of South Australia (UniSA) tested black phosphorus-based nanotechnology as an advanced infection treatment and wound healing therapeutic.
Black phosphorus is the most stable form of phosphorus - a mineral that is naturally present in many foods - and, in an ultra-thin form, degrades easily with oxygen, making it ideal for killing microbes.
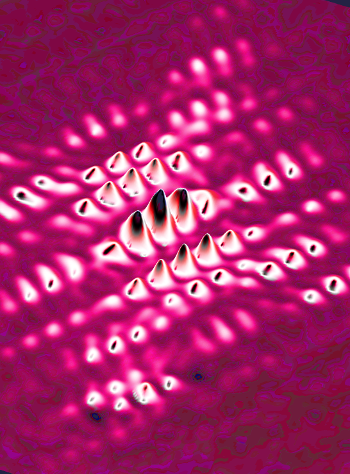
As the nanomaterial breaks down, its surface reacts with the atmosphere to produce what are called reactive oxygen species. These species ultimately help by ripping bacterial cells apart.
The new study tested the effectiveness of nano-thin flakes of black phosphorus against five common bacteria strains, including E. coli and drug-resistant golden staph.
Results show it effectively treated infections, killing over 99 per cent of bacteria, without damaging other cells in biological models.
The treatment achieved comparable results to an antibiotic in eliminating infection and accelerated healing, with wounds closing by 80 per cent over seven days.
The superbug-killing nanotechnology developed internationally by RMIT was rigorously tested in pre-clinical trials by wound-healing experts at UniSA.
RMIT has sought patent protection for the black phosphorus flakes including its use in wound healing formulations, including gels.
RMIT co-lead researcher, Professor Sumeet Walia, said the study showed how their innovation provided rapid antimicrobial action, then self-decomposed after the threat of infection had been eliminated.
“The beauty of our innovation is that it is not simply a coating – it can actually be integrated into common materials that devices are made of, as well as plastic and gels, to make them antimicrobial,” said Walia from RMIT’s School of Engineering.
A previous study led by RMIT revealed that black phosphorus was effective at killing microbes when spread in nano-thin layers on surfaces used to make wound dressings and implants such as cotton and titanium, or integrated into plastics used in medical instruments.
The team wants to collaborate with potential industry partners to develop and prototype the technology.
More details are accessible here.








 Print
Print